Uncommon commonalities: Applying behavioral economics to medication adherence
By Dale Hanna
Ask any group of healthcare providers why patient outcomes fall short of expectations, and they will cite patient adherence to treatment as a major culprit. And they'd be right.
An estimated 50 to 60 percent of patients with chronic illness skip their medications, alter doses, or stop their treatment altogether in the first year. The result is a huge burden on the U.S. healthcare system—approximately 125,000 preventable deaths and $290 billion are directly attributed to non-adherence each year.1
For years, healthcare organizations, researchers, and pharmaceutical companies have been trying to uncover the root causes of non-adherence. Why do people skip doses or stop taking medications that they know will treat disease, help prevent complications, and improve their quality of life? Surprisingly, it could be the same reason many people fail to exercise even though they know the benefits, or why others choose junk food even when they know it's bad for them. Why do humans choose options that are second best for our health when we have the knowledge and ability to make better, more informed choices?
Tapping into behavioral economics
Gaining a deeper understanding of why patients do the things they do has become the holy grail for developing effective patient services to support medication adherence. In fact, behavioral science plays an increasing role in how the most advanced patient support services are being delivered and designed today.
Behavioral economics, a field that uses psychological insight into human behavior to explain economic decision-making, may just hold the key to solving the medication adherence problem. One of the underlying theories of behavioral economics is that human beings are all intrinsically irrational—we persistently make bad decisions despite knowing they aren't best for us.
That irrationality means people often take actions or make decisions that conflict with their long-term interests, including not taking their medication as prescribed. Applying this theory to interventions designed to encourage patients to stick with their treatment regimens offers great potential to steer patients in the right direction, helping them build sustainable habits when it comes to their healthcare.
"One of the underlying theories of behavioral economics is that human beings are all intrinsically irrational–we persistently make bad decisions despite knowing they aren't best for us."
Understanding the uncommon commonalities
While behavioral economics helps explain the patient's decision-making process, it's still important to understand the contributing factors. There's a game used as an icebreaker or team-building exercise called “Uncommon Commonalities." The goal: to have the group of participants discover what they have in common among a list of characteristics that are somewhat unique, or uncommon.
Looking at a group of non-adherent patients through this lens, the commonality they share is the irrational behaviors that contribute to non-adherence. But as individuals, each person has a unique set of other barriers — the uncommon factors. These also link them by causing them to struggle with treatment adherence.
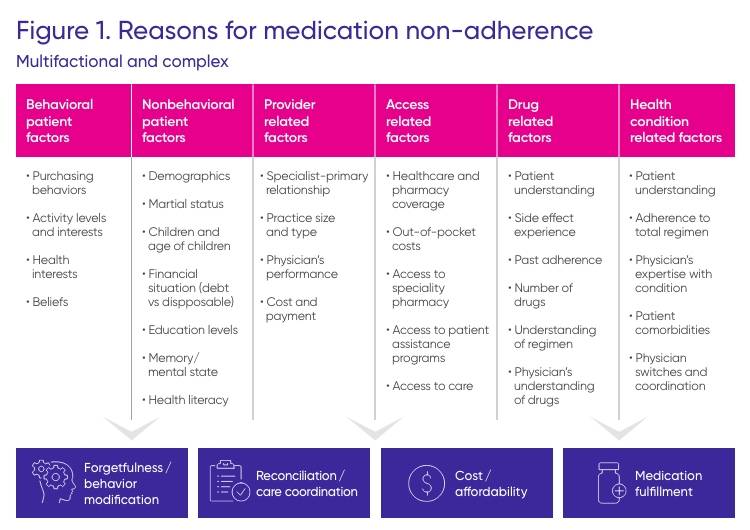
Myriad individual factors can impede a person's ability to take their medicine as prescribed. These barriers can include:2
- Cost. If patients cannot afford their medication, they may try to offset the cost by reducing the prescribed dosage and frequency or not filling the prescription at all.
- Misunderstanding. Patients may not understand the need for the medicine, the side effects, or how long it will take to see results.
- Multiple medications. More medications and higher dosing frequencies increase the likelihood for barriers that will influence a patient's ability to initiate or remain on treatment as prescribed.
- Lack of symptoms. Patients may feel a medication is ineffective if they don't feel a difference when starting or stopping the therapy.
- Negative beliefs. Patients may fear potential side effects, worry about becoming dependent, have concerns that the medication will disrupt their life, or feel their doctor does not understand them.
- Mental health issues. Depression and anxiety can cause patients to struggle with taking their medications.
The underlying factors that actually contribute to non-adherence can go far deeper than just these barriers, extending to multiple dimensions as outlined in Figure 1 below.
Closing the medication adherence gap
When it comes to developing patient support initiatives for treatment adherence, it's crucial to acknowledge that patients are human. They can make irrational health decisions and have a host of individual factors affecting their ability or willingness to follow through with prescribed therapy.
As such, there's no such thing as a one-size-fits-all approach to adherence support programs. It's important to focus on patient-centered models by creating resources for patients that provide the right behavioral nudge to lead them toward health improvement. A holistic, patient-centered approach can help close adherence gaps by empowering patients to participate in their own treatment journeys, assisting them with overcoming barriers, and promoting long-term behavior changes.
1. Annals of Internal Medicine. Interventions to Improve Adherence to Self-Administered Medications for Chronic Diseases in the United States: A Systematic Review. 4 December 2012. Accessed June 11, 2019 at: http://annals.org/aim/fullarticle/1357338/interventions-improve-adherence-self- administered-medications-chronic-diseases-united-states.
2. 8 reasons patients don't take their medications. American Medical Association. 6 October 2012. Accessed June 12, 2019 at: https://www.ama-assn.org/delivering-care/patient-support-advocacy/8-reasons-patients-dont-take-their-medications.
In part two of our Uncommon Commonalities series, discover further insights into developing effective adherence strategies, including the components that are critical during support program design. Sign up for email updates below to receive a notification when part two is available.





