The Power of Patient Activation: Part One
By AmerisourceBergen
Medication adherence is a primary determinant of treatment success. Yet, only 50 percent of patients with chronic conditions take their medications as prescribed.1 Non-adherence costs the healthcare system between $100-$289 billion annually and is associated with nearly 125,000 deaths and 10 percent of hospitalizations.2
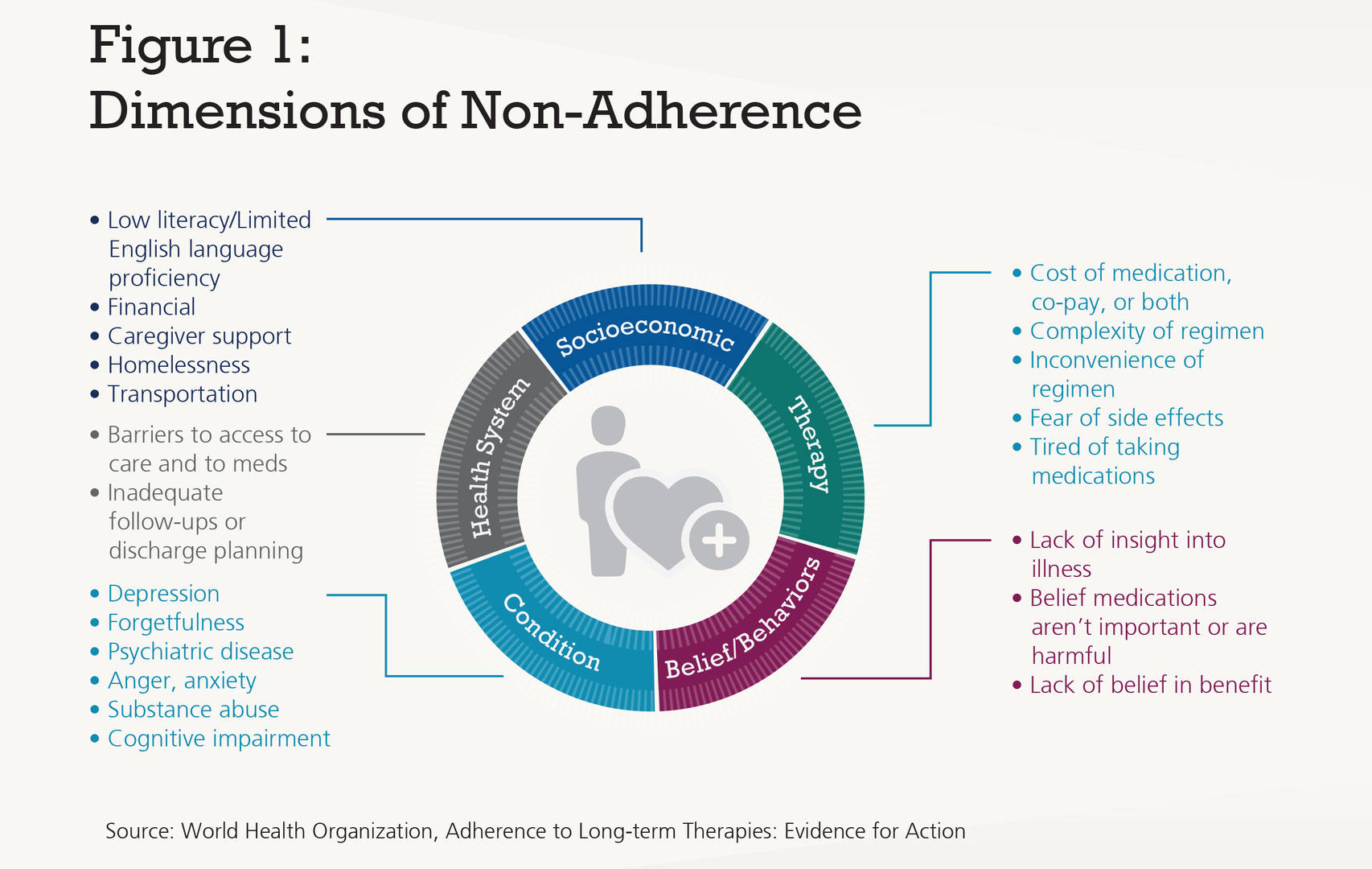
The reasons for non-adherence vary widely and often change over the course of a patient’s treatment journey. Causes of non-adherence include social and economic factors; patients’ perceptions, motivations and levels of physical/cognitive impairment; issues related to the specific medication therapy; the medical condition being treated; and the patient’s healthcare system. The vast landscape of factors contributing to non-adherence has been aggregated by the World Health Organization as shown in in Figure 1 below.3 Identifying a patient’s specific adherence barriers and developing an individualized care plan with short- and long-term goals are essential to improving outcomes. The key to unlocking better outcomes is putting patients at the center of treatment and support and empowering them to be active within their own health journey.4

A Complex Problem
Medication non-adherence is a complex issue to solve because there is potentially a combination of many product- and patient-specific factors that can impact whether a person takes their medication as prescribed. Affordability, adverse effects and lack of education around medication regimen are widely known drivers of poor adherence. But what about the hidden factors—or combination of factors—that can only be discovered through personalized interactions?
These factors might include a combination of the patient’s overall health literacy or understanding of the severity of their condition and ability to get to treatment sites on a regular basis. For example, just 53 percent of adults have intermediate health literacy (i.e., can read instructions on a prescription label and determine what time to take medication).5 Socioeconomic characteristics of the patient, such as gender, age, level of education and level of income also play a role. These contributors are often more critical to address than product-centric factors.Patient-specific Reasons for Medication Non-adherence
- Just 53% of adults have intermediate health literacy6
- 24% of patients cite forgetfulness7
- 14% have the perception that the prescribed drug would have little effect on their disease8
Historic Approaches to Improving Adherence
Many adherence programs employ a one-size-fits-all approach that focuses on building product-centric engagement, with the belief that educating the patient on the drug’s efficacy, safety and dosing instructions is enough to keep them adherent and address the questions they may have.Under a product-centric adherence program, each patient might receive calls at pre-specified intervals (i.e., days 3, 10, 30, 60 and 90), and each patient is given the same information on the product, condition and side effect management. If a patient has access questions and financial challenges, outreach can be made to the patient support team to obtain clarity on benefits and financial support services. Compliance programs that take this approach might be built on the belief that access and financial barriers are the only challenges patients face, and that by addressing these hurdles, the patient will remain adherent.
However, these product-centric programs may fail to unearth the true root causes of patient non-adherence and the social and behavioral determinants that often accompany them. Patients need more than well-intentioned, prescriptive advice. What is needed is an approach that addresses the complex interaction of motivations, health system barriers, perceptions of therapy benefits, socioeconomic and behavioral influences, and readiness to change. Taking a patient-centered approach matches a patient’s medication adherence needs with specifically tailored tools and strategies.


