Upping the Game
By Kristin Chambers
A new paradigm
As healthcare reimbursements move from fee-for-service (FFS) to value-based payments, the pressure has never been greater to demonstrate the quality of patient care. In response, drug manufacturers, health systems and payers are simultaneously seeking new ways to improve value and patient outcomes, while protecting reimbursements.
Indeed, the patient-minded model of care has arrived. Now more than ever, key healthcare players must communicate and work closely together to succeed. That means leaving the traditional FFS model behind, because it drives fragmentation and doesn't support transparency and collaboration among providers and channel partners.
How can manufacturers collaborate with health systems to positively affect patient-minded care? How can health systems and manufacturers share information and expertise to improve the patient experience and outcomes?
These are the challenges of our times. And for manufacturers, the solution begins with understanding.
Three ways to closer collaboration
Traditionally, manufacturers have collaborated with health systems by seeking to introduce drugs into their formularies. While still valid, that approach is no longer enough. Forward-thinking manufacturers-as well as payers and providers-should be thinking more broadly about other ways to collaborate, such as improving medication adherence and developing transitional care initiatives that ensure the continuity of care.
By taking a more holistic approach that embraces the patient's experience across the entire care continuum, we can more effectively achieve the better outcomes and higher patient satisfaction levels that are the primary goals of a patient-minded care model.
Here's a closer look at three anchors of closer collaboration: medication access for patients, medication adherence and transitional care.
1. Medication access for patients
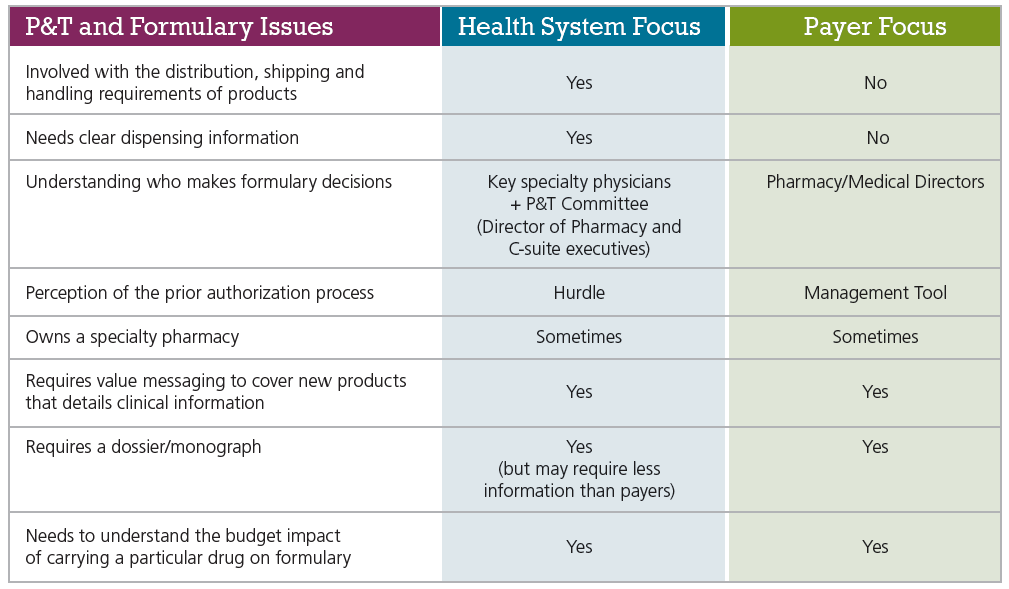
How can manufacturers better position their drugs to be included in provider formularies for improving patient care? The first step is recognizing the differences in how health systems and payers approach P&T (pharmacy and therapeutics) and formulary decisions. For example, health systems may require less drug information than payers and have different operational considerations, such as a focus on distribution, handling and dispensing.Understanding these key issues can help manufacturers more effectively present the value of their products to improve patient outcomes while efficiently managing costs. As a starting point, here are many of the major P&T and formulary issues and how each impacts health systems and payers (chart below).
Presenting manufacturer value to health systems
To demonstrate an understanding of formulary processes and how to add value through close collaboration, manufacturers can follow these two steps:
Determine the P&T review process in the health system:
- Representation: Who is involved in the review process? What is the mix of physicians, pharmacists, C-suite executives (for example, the CFO and CNO), safety officer and other health professionals?
- Review: How often are the formulary's therapeutic classes reviewed that are relevant to your products?
- Budget Impact: Remember to consider more than just the drug acquisition costs. What are the health system's other considerations, such as reimbursement performance, sites of care, he impact of bundled payments, special handling requirements and specific patient needs?
Discuss best practices:
- Health system experience: Based on the health system's collaboration with other manufacturers, what best practices has it used to support the P&T and formulary review process?
- Timing: What is the drug's launch date? How soon could prescribers and their patients have access to your product (taking any FDA approval review into account or the actual launch date versus approval date)? Are there any special distribution and/or handling considerations?
2. Medication adherence
Non-adherence can lead to significant revenue losses for manufacturers, as well as poor patient outcomes. Non-adherence can also lead to a false impression that the drug isn't performing as expected (when in fact, the negative outcome is the result of the medication not being taken as prescribed).
In a time when patent expirations outnumber breakthrough discoveries-and payers demand tighter cost containment and lower prices-forward-thinking manufacturers should seek new ways and channels to help improve adherence and overall patient care.
That means looking beyond traditional approaches, such as free drugs, direct-to-consumer co-pay assistance and couponing at the point-of-sale. In addition, manufacturers will want to seek closer collaboration with health systems, because they have the direct patient contact that drug makers typically lack. Indeed, providers have an important financial stake in patient outcomes as well, given how reimbursements are shifting toward a value-based model.
So what is the root cause of non-adherence-and how can manufacturers collaborate with health systems to help reverse the trend? A lack of adherence can begin with patient behaviors, such as:
- Not understanding the disease and its impact on health
- Lack of understanding of why taking the drug as prescribed is important
- Forgetfulness
- Lack of convenience, because the pharmacy is "out of the way"
- Not being proactive and taking ownership of their own health
For in-patients, the problem of non-adherence can literally begin at admission and continue beyond discharge. If the correct set of medication instructions aren't followed every step of the way, the potential for non-adherence grows.
At Xcenda and PHS, we believe there is a need for stronger communication, to better educate and enlighten patients on the value of taking their medications as prescribed. Going forward, patient adherence initiatives must build a stronger bridge of communication that connects patients more closely with providers, payers and manufacturers.
In a patient-minded world, we must all recognize that patients who are more informed will be more proactive and take greater ownership of their health. When manufacturers are proactive themselves in not only measuring adherence-but also promoting education-the result will be healthier, happier and more satisfied patients. We can work closely together to create this brighter future. In the end, everyone will benefit.
3. Transitional care: avoiding 30-day readmissions
As health systems plan to better manage patient health "outside the four walls of the hospital," how can manufacturers help them address a critical aspect of transitional care: avoiding 30-day readmissions and their penalties?
The maximum penalty for 30-day readmissions is now in force: 3% of reimbursements. As a result, readmissions are one of the hottest topics in healthcare today. Health systems are forming 30-day readmissions reduction teams-and many administrators and clinicians are seeking third-party guidance to develop an effective solution.
Manufacturers can become part of the solution by collaborating with providers to combine six best practices of transitional care into a single, sustainable solution. These best practices are:
- On-site, full-time program management
- Medication reconciliation
- After-hospital care planning
- Managing skilled nursing and LTC transitional care
- Maximizing transitional care payments to providers
- Using a transitional care program to promote the health system's brand
A catalyst for better outcomes
Together, Xcenda and PHS provide a complete, end-to-end consulting solution to help facilitate closer collaborations among drug manufacturers, health systems and payers. Xcenda focuses upstream on manufacturers and payers, while PHS focuses downstream on health systems.
Through these collaborations, health systems benefit from education and advocacy around key industry trends such as 340B drug pricing, risk-based payment models and adjusting service lines to accommodate the rapid expansion of non-acute sites of care. At the same time, health systems share their own market insights and priorities with manufacturers to help guide product innovation, facilitate demand planning and optimize supply chain processes.
Together, we can facilitate the merger of all stakeholders in the value chain—devising innovative solutions that positively affect patient access and outcomes. Contact us when you're ready to create your own patient-minded care solution.




