Insight Series: Value of Patient Support Programs for Specialty Medications in Canada
By AmerisourceBergen
Gaps in Canadian Healthcare System for Specialty Medications
Many people assume that the cost of all healthcare services are covered in Canada, but this does not apply to all services for specialty medications. Clinical services are required for many specialty medications, including infusion or injections in clinics or via home care, and these services may not be covered by public or private payers. Further, specialty medications often haveunique administration requirements that necessitate additional or customized training, and ongoing support of patients and their caregivers, for example: mothers who have to provide regular injections to their young children may need more frequent advice or even respite support; patients prescribed medications dosed by weight may need support for precise dosing administration; and some patients may need more contact with a healthcare professional (HCP) as their specialty medication is being titrated. Regular disease management support, including patient and caregiver education and frequent touch points, cannot always be provided readily by HCPs due to the administrative and time constraints of clinical practice, and there is often limited support available outside of physician visits, or limited knowledge of the additional public support available.
Many people assume that the cost of all healthcare services are covered in Canada, but this does not apply to all services for specialty medications.
The journey to gain access to a specialty medication is daunting for patients, particularly when they are quite ill, and there is little support to navigate this difficult process. Lack of knowledge of public and private reimbursement mechanisms and criteria, and coordination of benefits; and the complexity of paperwork and testing requirements, can cause delays in treatment and much anxiety and fear amongst patients and caregivers. Additionally, Special Authorization for specialty medications is generally required for public and private reimbursement decision-making, and the process is complex and time-consuming for HCPs and patients alike.
Medication non-adherence leads to sub-optimal health outcomes, increased healthcare resource utilization, and increased direct and total medical costs; however, the healthcare system cannot always provide the support that many patients need to stay on therapy and refill their prescriptions. The WHO reported that adherence among patients with chronic diseases averages only 50% in developed countries1, and up to 30% of patients fail to fill a new prescription.2,3 Interventions that can address the possible risk factors for non-adherence and sustain patient medication adherence and persistence are needed to reduce the economic and health burdens of complex chronic diseases, but services to support HCP instructions outside of clinic visits are not provided by public or private payers.
Currently, healthcare-related data necessary to determine how a patient is responding to their specialty medication is fragmented and inconsistent as it comes from many different sources. A consolidated view is not readily available to HCPs, e.g. trends in Health Assessment Questionnaire (HAQ) for rheumatoid arthritis and lab values, and there is no data available to a physician to determine whether a prescription has been filled or refilled. A more robust, formal approach to collecting data is important to help facilitate HCP access to patient data, and to enable the collection of health outcomes data that would benefit payer decision-making.
PSPs Provide Value to Help Fill the Gaps in the Healthcare System
Manufacturer-supported PSPs were created over 15 years ago to support patient access to complex medications. Now PSPs provide a more holistic approach to patient, caregiver, and HCP support when specialty medications are prescribed, including: reimbursement navigation; clinic and nursing support (infusion and injection administration/ training); patient education and counseling; risk management and adherence; specialty pharmacy and logistics services; and connection to other social support services. PSPs fill the gaps in services not readily available in the current healthcare system to help optimize health outcomes and value in patient-focused care. As a result, PSPs have demonstrated a positive impact on patient adherence, and clinical and economic outcomes.4,5
PSPs fill the gaps in services not readily available in the current healthcare system to help optimize health outcomes.
PSPs support patient disease management by providing rapid access to specialty drug administration and education. PSP clinic and field nurses administer injections and infusions, patient self-injection training, and rigorous safety monitoring, in the convenience of local private clinics or in patients’ homes. PSP nurse case managers also provide education, and ongoing lifestyle, health and wellness support to patients via frequent touch points.
Reimbursement specialists have experience with the complexity of drug reimbursement navigation, and support patients through their entire journey to help ensure patients get on drug faster and maximize their coverage. Changes in health care policy poses challenges for reimbursement, as do the forms, policies and requirements that can change and vary greatly by provincial and private payers; however, PSP reimbursement specialists are experts in the payer landscape and the technology required to expedite the process. They support patients and HCPs in completing all payer forms, submissions, and escalation of denials. Field case managers also support physicians and nurses in their clinic by helping to coordinate testing and appointments, and to support the administrative burden of the reimbursement process.
PSP nurse case managers are integral in supporting patient adherence to help optimize treatment outcomes. They are a single point of contact for each patient to support: patient health literacy; understanding of the patient’s treatment regimen and expected results; coordination of drug ordering and delivery so there is no gap in their treatment; and to follow up with the patient to ensure they are adhering to their treatment plans. Nurse case managers provide motivation and knowledge to empower patients, assess patients for non-adherence risk factors, and customize patient touch points based on patient need. Touch points can include a variety of mediums, including regular phone calls, and technology-based adherence interventions. Additionally, nurse case managers can connect patients and families to support services that they may not be aware of, such as, patient advocacy groups, government-funded programs, social workers, etc. If a fully integrated model is used, the access to pharmacy data can also help to quantify patient non-adherence, and nurse case managers can provide this information via a regular feedback loop to the prescribing physician.
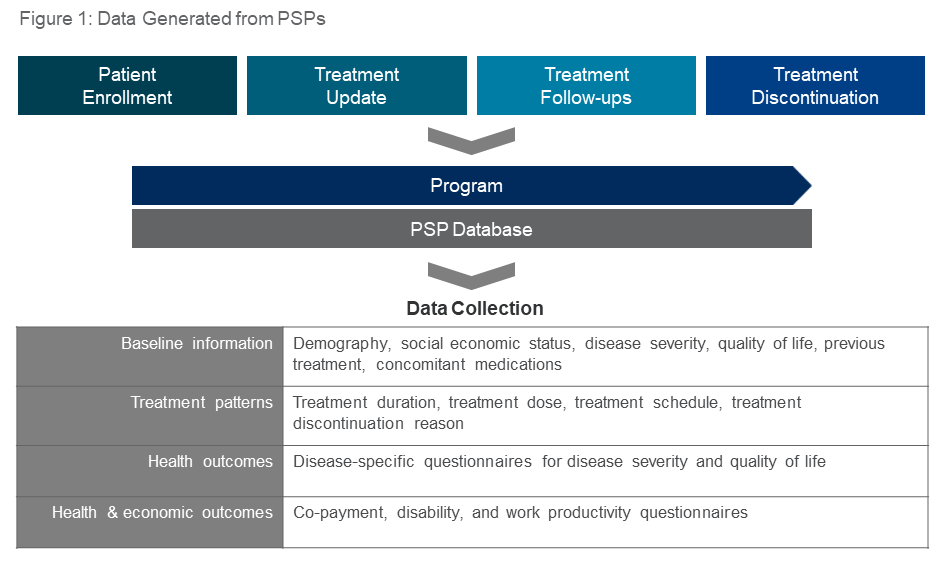
Healthcare-generated data obtained by PSPs can provide important insights for HCPs, payers, and manufacturers. Through on-line PSP portals, HCPs can readily access consolidated patient-specific data, such as disease scores, and medication adherence and persistence. As payers look to manufacturers to present real world evidence, patient data from PSPs can be used to assess treatment patterns, and health and economic outcomes (Figure 1). A variety of patient-reported health outcome studies can be performed, including: quality of life, product effectiveness, treatment adherence, safety, health resources utilization, and indirect costs such as productivity loss, out-of-pocket costs and the cost of informal care. From a manufacturer perspective, these health outcomes studies can align to global strategy and be leveraged to support reimbursement and listing.
PSPs provide value by helping patients to better manage chronic diseases and optimize complex treatment by filling the gaps in services that are not provided in the current healthcare system. The future focus of PSPs will be on an evolution in integrating the process and efficiencies for patients, HCPs, payers, and manufacturers that will offer increased value to all stakeholders. By offering a more seamless experience for patients and HCPs, and greater cost effectiveness through investment in digital technology, connectivity to healthcare systems, and the provision of health outcomes data, PSPs will be even more able to maximize patient health outcomes.
This article is one in a series provided by Innomar Strategies to update manufacturers on relevant changes and new information in the specialty pharmaceutical marketplace.
References:
1. Sabaté E. Adherence to Long-Term Therapies: Evidence for Action, World Health Organization, Geneva, Switzerland, 2003. Accessed 7 March 2018
2. Fischer MA et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25(4):284-90. Accessed rel="noopener noreferrer" 7 March 2018 at
3. rel="noopener noreferrer" Tamblyn R et al. The incidence and determinants of primary nonadherence with prescribed medication in primary care: A cohort study. Ann Intern rel="noopener noreferrer" Med. 2014;160(7):441-450. Accessed rel="noopener noreferrer" 9 March 2018
4. rel="noopener noreferrer" Ganguli A et al. The impact of patient support programs on adherence, clinical, humanistic, and economic patient outcomes: a targeted systematic rel="noopener noreferrer" review. Patient Pref Adherence. rel="noopener noreferrer" 2016;10:711-25. Accessed rel="noopener noreferrer" 9 March 2018
5. Rubin DT et al. Impact of patient support program on patient adherence to adalimumab and direct medical costs in Crohn’s disease, ulcerative colitis, rheumatoid arthritis, psoriasis, psoriatic arthritis, and ankylosing spondylitis. J Manag Care Spec Pharm. 2017;23(8):859-867. Accessed 9 March 2018



